Health Topics
- Coronavirus
- Ebola
- Flu
- Conjuctivitis
- FoodBorne Illness
- EBV
- MONO
- Meningitis
- MRSA/Staph
- Norovirus
- Pharyngitis
- Common Cold
- STIs/STDs
- Stress
Novel Coronavirus 2019 (COVID-19)
 Ebola Virus
Ebola Virus
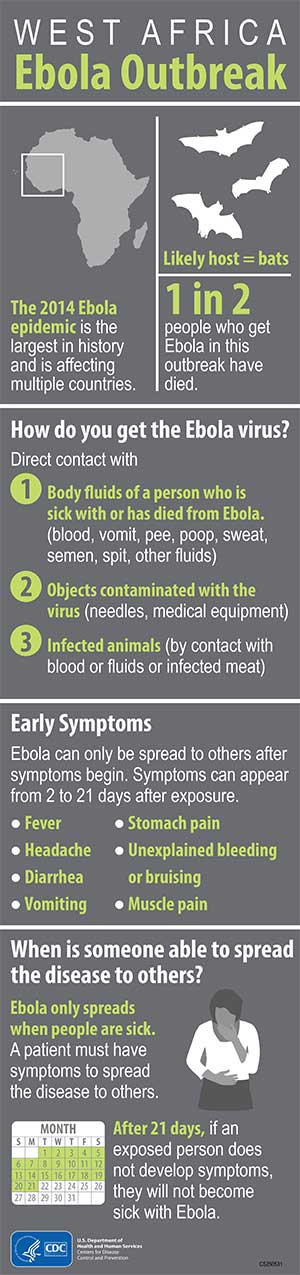
Transmission: Ebola then spreads through human-to-human transmission via direct contact (through broken skin or mucous membranes) with the blood, secretions, organs or other bodily fluids of infected people, and with surfaces and materials (e.g. bedding, clothing) contaminated with these fluids.
Symptoms: The incubation period, that is, the time interval from infection with the virus to onset of symptoms is 2 to 21 days. Humans are not infectious until they develop symptoms. First symptoms are the sudden onset of fever fatigue, muscle pain, headache and sore throat. This is followed by vomiting, diarrhea, rash, symptoms of impaired kidney and liver function, and in some cases, both internal and external bleeding (e.g. oozing from the gums, blood in the stools). Laboratory findings include low white blood cell and platelet counts and elevated liver enzymes.
Risk: Healthcare providers caring for Ebola patients and the family and friends in close contact with Ebola patients are at the highest risk of getting sick because they may come in contact with the blood or body fluids of sick patients. People also can become sick with Ebola after coming in contact with infected wildlife.
Prevention: Gloves and appropriate personal protective equipment should be worn when taking care of ill patients at home. Regular hand washing is required after visiting patients in hospital, as well as after taking care of patients at home.
How do I protect myself against Ebola? If you must travel to an area affected by the 2014 Ebola outbreak, protect yourself by doing the following:
- Wash hands frequently or use an alcohol-based hand sanitizer.
- Avoid contact with blood and body fluids of any person, particularly someone who is sick.
- Do not handle items that may have come in contact with an infected person’s blood or body fluids.
- Do not touch the body of someone who has died from Ebola.
- Do not touch bats and nonhuman primates or their blood and fluids and do not touch or eat raw meat prepared from these animals.
- Avoid facilities in West Africa where Ebola patients are being treated. The U.S. Embassy or consulate is often able to provide advice on medical facilities.
Seek medical care immediately if you develop fever, headache, muscle pain, fatigue, diarrhea, vomiting, stomach pain, or unexplained bruising or bleeding.
Limit your contact with other people until and when you go to the doctor. Do not travel anywhere else besides a healthcare facility.
For more information:
http://www.who.int/mediacentre/factsheets/fs103/en/
http://www.cdc.gov/vhf/ebola/
http://www.cnn.com/2014/04/11/health/ebola-fast-facts/
In the wake of the Ebola epidemic/outbreaks in West Africa, Middle Georgia State is following the " Advice for Colleges, Universities, and Students about Ebola in West Africa" document issued by the Centers for Disease Control.
Based on this advice, individuals are asked to:
- Avoid non-essential travel including education-related travel to countries with a Centers for Disease Control (CDC) Level 3 warning for Ebola.
- Closely monitor travel advisories for your destination: wwwnc.cdc.gov/travel/notices / travel.state.gov
- Review GA Department of Public Health information regarding screening of travelers returning from Ebola–affected countries at dph.georgia.gov/screening-travelers-atlantas-airport.
- Contact Shawn Douglas, chief of police, at 478.471.2414 or for latest advisories and guidance from the CDC, the Georgia Ebola Response Team, and the Department of Public Health.
Additional information concerning Ebola may be found at www.cdc.gov/vhf/ebola/about.html.
Ebola is a severe, often fatal disease that spreads through direct contact with an infected person's blood or their body fluids such as feces, saliva, urine, vomit, and semen. Ebola can also spread by direct contact with objects contaminated with an infected person's blood or body fluids or by direct contact with infected animals.
- Prior to returning to campus, contact Shawn Douglas, chief of police, at or 478.471.2414.
- Be prepared to respond to questions related to your travel, potential exposure history, and whether you are experiencing signs and symptoms of Ebola virus disease such as fever, headache, fatigue, muscle pain, diarrhea, vomiting, abdominal pain or unusual bruising or bleeding.
- If you are symptom free during the 21 day monitoring period, continue your routine activities including attending class and work.
Additional information concerning Ebola may be found at www.cdc.gov.
Flu Season
As the flu season approaches it is important that you know how to keep yourself safe from getting sick. As a college student, getting sick can result in a grade reduction or even failure of a class. As an employee, the flu will mean lost work hours and possibly pay. This can have a huge impact on your career plans. Don’t let that happen to you. Following these 5 simple ideas will reduce the chances that flu will catch you off guard.
1. Get the flu vaccine
According to the CDC the single most effective way to keep from contracting the flu is to get the annual flu vaccination. Each year the flu virus mutates and a new vaccine is developed to target the new strain. Many people report not getting the vaccine because it “makes them sick”, but the truth is that the vaccine makes it easier in the short term for you to catch the common cold. To prevent this use the remainder of the tips below.
2. Clean your hands
Some think the dirtiest part of the human body is the mouth but it very well could be your hands. Your hands touch everything around (including your mouth) and as a result pick up viruses, bacteria, mold and many other dirty stuff. When your hands touch moist areas of your body such as your eyes, nose and mouth, you transfer the “gross stuff” to a nice warm and cozy place for it to breed. And then… you get an infection. Washing your hands with soap and water is the easiest and most effective way to prevent this pattern of contracting an infection.
3. Don’t touch your eyes, nose and mouth
As noted above, when you touch your mouth you put the bacteria, or virus where it can grow and spread more easily. You transfer the bacteria into your system where your body must fight it off. To avoid the fight don’t introduce it in the first place. Keep your hands and fingers (and toes for that matter) away from your face.
4. Avoid close contact with others
When people are sick they harbor the infective material on their clothes, skin and actually in their breath. If you are close to them you can pick up some of this infective material and introduce it to your own system. For this reason, doctors have found that the elbow bump and fist bump are better than a handshake. It is not intended to be antisocial but to reduce the contact between people and thus decrease the spread of illness.
5. Stay Well
Yes, staying well decreases that you will get sick. The CDC suggests practices that boost your immune system rather than reducing it. This includes getting plenty of sleep, water, vitamins, nutritious food and physical activity. Your immune system is a machine, and when it does not have the necessary tools to function, it fails. Failure of your defenses will leave you vulnerable to getting sick.
Remember if you want to keep from catching the flu you must not be caught off guard. Following these principles will reduce your risk of infection and improve your chances of having a successful semester.
Adapted from CDC.gov http://www.cdc.gov/flu/protect/habits.htm
Conjunctivitis
Description: Conjunctivitis is often called "pink eye" or "red eye" because it can cause the white of the eye to take on a pink or red color. Signs and symptoms of pink eye can vary but typically include redness or swelling of the white of the eye.
Conjunctivitis is an inflammation or infection of the conjunctiva, the thin transparent layer of tissue that lines the inner surface of the eyelid and covers the white part of the eye. Conjunctivitis, often called “pink eye,” is a common eye disease, especially in children. It may affect one or both eyes. Some forms of conjunctivitis can be highly contagious and easily spread in schools and at home. While conjunctivitis is usually a minor eye infection, sometimes it can develop into a more serious problem.
Conjunctivitis may be caused by a viral or bacterial infection. It can also occur due to an allergic reaction to irritants in the air like pollen and smoke, chlorine in swimming pools, and ingredients in cosmetics or other products that come in contact with the eyes. Sexually transmitted diseases like Chlamydia and gonorrhea are less common causes of conjunctivitis.
People with conjunctivitis may experience the following symptoms:
- A gritty feeling in one or both eyes
- Itching or burning sensation in one or both eyes
- Excessive tearing
- Discharge coming from one or both eyes
- Swollen eyelids
- Pink discoloration to the whites of one or both eyes
- Increased sensitivity to light
For more information:
http://www.cdc.gov/conjunctivitis/
PODCAST on Pinkeye - "What to Do"
http://emedicine.medscape.com/article/797874-overview
Foodborne Illness
Foodborne illness is the sickness that results from eating foods that are contaminated with harmful bacteria and other microorganisms. Although you may not see, smell or taste these "bugs", under the right conditions, they may be present on the foods when they're purchased or get into food during preparation, cooking, serving or storage.
Common symptoms of foodborne illness include diarrhea, abdominal cramps, fever, headache and vomiting. These symptoms may come on as early as a half hour after eating contaminated food or may not develop for up to two weeks. They usually last only a day or two, but in some cases can persist a week or more. For most healthy people, foodborne illnesses are neither long lasting nor life threatening. However, the consequences can be severe and may require hospitalization and even lead to death in the very young, the very old and those with weakened immune systems.
What happens in the body after the microbes that produce illness are swallowed?
After the microbes are swallowed, there is a delay, called the incubation period, before the symptoms of illness begin. This delay may range from hours to days, depending on the organism, and on how many of them were swallowed.
During the incubation period, the microbes pass through the stomach into the intestine, attach to the cells lining the intestinal walls, and begin to multiply there.
Some types of microbes stay in the intestine, some produce a toxin that is absorbed into the bloodstream, and some can directly invade the deeper body tissues. The symptoms produced depend greatly on the type of microbe.
Numerous organisms cause similar symptoms, especially diarrhea, abdominal cramps, and nausea. There is so much overlap that it is rarely possible to say which microbe is likely to be causing a given illness unless laboratory tests are done to identify the microbe, or unless the illness is part of a recognized outbreak.
Epstein-Barr virus (EBV)
Epstein-Barr virus (EBV), also known as human herpesvirus 4, is a member of the herpes virus family. It is one of the most common human viruses. EBV is found all over the world. Most people get infected with EBV at some point in their lives. EBV spreads most commonly through bodily fluids, primarily saliva. EBV can cause infectious mononucleosis, also called mono, and other illnesses.
Symptoms
- fatigue
- fever
- inflamed throat
- swollen lymph nodes in the neck
- enlarged spleen
- swollen liver
- rash
Mononucleosis
Infectious mononucleosis (commonly called mono) is a viral disease that affects the throat, lungs, liver and lymphatic system. It usually affects children and young adults from 12 to 40 years old. Mono is caused by the Epstein-Barr virus and is passed from person to person by close contact, such as kissing and sharing eating utensils or food.
Symptoms
- Fever
- Sore throat
- Appetite loss
- Fatigue
- Headaches
- Muscle aches
- Swollen lymph glands, usually in the neck, underarms, or groin
- Enlarged spleen
- Enlarged liver
- Jaundice with yellow skin and eyes
Not all symptoms are present in every case.
https://www.uhs.uga.edu/healthtopics/mononucleosis.html
http://www.nlm.nih.gov/medlineplus/infectiousmononucleosis.html
http://www.cdc.gov/epstein-barr/about-mono.html
Meningitis
Description: Meningitis is a disease caused by the inflammation of the protective membranes covering the brain and spinal cord known as the meninges. The inflammation is usually caused by an infection of the fluid surrounding the brain and spinal cord. Meningitis may develop in response to a number of causes, usually bacteria or viruses, but meningitis can also be caused by physical injury, cancer or certain drugs.
Transmission:
- Bacterial: Bacterial meningitis is contagious. The bacteria are spread through the exchange of respiratory and throat secretions (i.e., kissing).
- Viral: Enteroviruses, the most common cause of viral meningitis, are most often spread from person to person through fecal contamination (which can occur when changing a diaper or using the toilet and not properly washing hands afterwards), but enteroviruses can also be spread via eye, nose, and mouth secretions (such as saliva, nasal mucus, or sputum), or blister fluid.
Symptoms:
Viral meningitis occurs more often than bacterial meningitis, and is milder. It usually occurs in the late summer and early fall. It most often affects children and adults under age 30.
Bacteria meningitis is an emergency. You will need immediate treatment in a hospital. Symptoms usually come on quickly, and may include:
- Fever and chills
- Mental status changes
- Nausea and vomiting
- Sensitivity to light (photophobia)
- Severe headache
- Stiff neck (meningismus)
Other symptoms that can occur with this disease:
- Agitation
- Bulging fontanelles in babies
- Decreased alertness
- Poor feeding or irritability in children
- Rapid breathing
- Unusual posture, with the head and neck arched backwards (opisthotonos)
Prevention:
Certain vaccines can help prevent some types of meningitis.
- Haemophilus vaccine (HiB vaccine) in children helps prevent one type of bacterial meningitis.
- The pneumococcal conjugate vaccine is now a routine childhood immunization. It is very effective at preventing pneumococcal meningitis.
- Household members and others in close contact with people who have meningococcal meningitis should receive antibiotics to prevent becoming infected.
The meningococcal vaccination is recommended for:
- Adolescents ages 11 - 12 and adolescents entering high school (about age 15) who have not already received the vaccination. A booster shot is given between age 16-18.
- All college freshmen who have not been vaccinated and are living in dorms.
- Children age 2 and older who do not have their spleen or who have other problems with their immune system.
- Those traveling to countries where diseases caused by meningococcus are very common (ask your doctor).
Some communities hold vaccination campaigns after an outbreak of meningococcal meningitis.
For more information:
http://www.cdc.gov/meningitis/index.html
http://www.nlm.nih.gov/medlineplus/ency/article/000680.htm
Community Associated MRSA and Staph Infections
Staph bacteria are one of the most common causes of skin infections in the United States. Most of these skin infections are minor such as pimples or boils and can be treated without antibiotics. However, staph bacteria can also cause serious infections, including those resistant to antibiotics, also known as MRSA (methicillin-resistant staphylococcus aureus).
Although most staph infections, including MRSA, occur most frequently in persons in hospitals, the infection can also be transmitted in settings outside hospitals and are referred to as community acquired MRSA.
MRSA in the community usually manifests as a skin infection such as a pimple or boil and worsens rapidly.
Staph infections and MRSA can be prevented by practicing good hygiene.
- Wash hands thoroughly using soap and water or an alcohol-based hand sanitizer.
- Keep cuts and scrapes clean and covered with a bandage until healed.
- Avoid contact with other people's wounds or bandages.
- Avoid sharing personal items such as towels or razors.
For more information:
https://www.uhs.uga.edu/healthtopics/staph.html
http://www.webmd.com/skin-problems-and-treatments/ss/slideshow-closer-look-at-mrsa
http://www.staph-infection-resources.com/info/mrsa-pictures/
http://www.emedicinehealth.com/mrsa_infection/article_em.htm
Norovirus
Norovirus is a very contagious virus. You can get norovirus from an infected person, contaminated food or water, or by touching contaminated surfaces. The virus causes your stomach or intestines or both to get inflamed (acute gastroenteritis). This leads you to have stomach pain, nausea, and diarrhea and to throw up.
Anyone can be infected with norovirus and get sick. Also, you can have norovirus illness many times in your life. Norovirus illness can be serious, especially for young children and older adults.
Norovirus is the most common cause of acute gastroenteritis in the United States. Each year, it causes 19-21 million illnesses and contributes to 56,000-71,000 hospitalizations and 570-800 deaths. Norovirus is also the most common cause of foodborne-disease outbreaks in the United States.
Norovirus spreads very easily and causes vomiting and diarrhea. There's no vaccine to prevent infection and no drug to treat it. Wash your hands often and follow simple tips to stay healthy.
Noroviruses are a group of related viruses. Infection with these viruses causes gastroenteritis (GAS-tro-en-ter-I-tis), which is inflammation of the stomach and intestines. This leads to stomach cramping, nausea, vomiting, and diarrhea.
Many Names, Same Symptoms
You may hear norovirus illness called "food poisoning" or "stomach flu." It is true that food poisoning canbe caused by noroviruses. But, other germs and chemicals can also cause food poisoning. Norovirus illness is not related to the flu (influenza), which is a respiratory illness caused by influenza virus.
Symptoms of norovirus infection usually include cramping, nausea, vomiting, and diarrhea.
Other, less common symptoms may include low-grade fever, chills, headache, muscle aches, and general sense of fatigue.
Norovirus illness is usually not serious. Most people get better in 1 to 3 days. But, norovirus illness can be serious in young children, the elderly, and people with other health conditions. It can lead to severe dehydration, hospitalization and even death.
You may get dehydrated if you are not able to drink enough liquids to replace the fluids lost from vomiting or having diarrhea many times a day. Symptoms of dehydration include a decrease in urination, a dry mouth and throat, and feeling dizzy when standing up. Children who are dehydrated may also cry with few or no tears and be unusually sleepy or fussy.
The best way to prevent dehydration is to drink plenty of liquids. Oral rehydration fluids are the most helpful for severe dehydration. But other drinks without caffeine or alcohol can help with mild dehydration. However, these drinks may not replace important nutrients and minerals that are lost due to vomiting and diarrhea.
Norovirus Spreads Quickly
Norovirus can spread quickly from person to person in crowded, closed places like nursing homes, daycare centers, schools, hotels, and cruise ships. Noroviruses can also be a major cause of outbreaks in restaurants and catered-meal settings if contaminated food is served.
The viruses are found in the vomit and stool of infected people. You can get it by
- Eating food or drinking liquids that are contaminated with norovirus
- Touching surfaces or objects contaminated with norovirus and then putting your hand or fingers in your mouth
- Having direct contact with a person who is infected with norovirus, for example, when caring for someone with norovirus or sharing foods or eating utensils with them
People with norovirus illness are contagious from the moment they begin feeling sick until at least 3 days after they recover. But, some people may be contagious for even longer.
Norovirus: No Vaccine and No Treatment
There is no vaccine to prevent norovirus infection. Also, there is no drug to treat people who get sick from the virus. Antibiotics will not help if you have norovirus illness. This is because antibiotics fight against bacteria, not viruses. The best way to reduce your chance of getting norovirus is by following some simple tips.
Protect Yourself and Others from Norovirus
1. Practice proper hand hygiene
Wash your hands carefully with soap and water, especially after using the toilet and changing diapers and always before eating or preparing food. If soap and water aren't available, use an alcohol-based hand sanitizer. These alcohol-based products can quickly reduce the number of germs on hands in some situations, but they are not a substitute for washing with soap and water.
2. Take care in the kitchen
Carefully rinse fruits and vegetables, and cook oysters and other shellfish thoroughly before eating them.
3. Do not prepare food while infected
People with norovirus illness should not prepare food for others while they have symptoms and for 2 days after they recover from their illness.
4. Clean and disinfect contaminated surfaces
After throwing up or having diarrhea, immediately clean and disinfect contaminated surfaces by using a bleach-based household cleaner as directed on the product label. If no such cleaning product is available, you can use a solution made with 5 tablespoons to 1.5 cups of household bleach per 1 gallon of water.
5. Wash laundry thoroughly
Immediately remove and wash clothing or linens that may be contaminated with vomit or stool. Handle soiled items carefully—without agitating them—to avoid spreading virus. If available, wear rubber or disposable gloves while handling soiled clothing or linens and wash your hands after handling. The items should be washed with detergent at the maximum available cycle length and then machine dried.
The best way to help prevent norovirus is to practice proper hand washing and general cleanliness.
http://www.cdc.gov/norovirus/index.html
http://www.cdc.gov/norovirus/about/overview.html
http://www.cdc.gov/features/norovirus/
http://www.cdc.gov/HAI/organisms/norovirus.html
Acute Pharyngitis in the College Health Setting
Pharyngitis accounts for 2% of visits to a doctor in the US and is due to a viral infection in ~80%of those instances. There is a wide range of viral culprits (rhino, adeno, coxackie, influenza, parainfluenza, herpes, and Epstein Barr (mono)). Each of these viral infections can cause a sore throat with or without other cold/flu symptoms. Treatment for sore throats of a viral origin is designed to decrease the symptoms while your body’s immune system eliminates the virus. These same strategies also improve symptoms of bacterial pharyngitis. Additionally antibiotic therapy is often included for the treatment of bacteria. The remaining document addresses the current clinical decision making philosophy of the CDC.
Diagnosis
Lab testing is not indicated in all patients with pharyngitis. Instead, all adults should be screened for the following:
- History of fever
- Lack of cough
- Tonsillar exudates
- Tender anterior cervical adenopathy
Patients with none or only one of these findings should not be tested or treated for GABHS.
Rapid streptococcal antigen test (RAT) is recommended for patients with 2 or more criteria, with antibiotic therapy restricted to those with positive test results.
Cultures are not recommended for routine evaluation of adult pharyngitis or for confirmation of negative results on rapid antigen tests if test sensitivity >80%.
Throat cultures maybe useful for outbreak investigation, monitoring rates of antibiotic resistance, or when other pathogens (e.g., gonococcus) are being considered.
https://www.uhs.uga.edu/healthtopics/CDC-UHC-Strep-Throat.pdf
http://www.nlm.nih.gov/medlineplus/ency/article/000655.htm
Upper Respiratory Infections
Upper respiratory infections, usually called "the common cold," may include sore throat, fever, headache, earache, sneezing, runny nose, congestion or cough. No specific treatment is available for the common cold since it is caused by a virus, but antibiotics can be prescribed for secondary bacterial infections.
People "catch" colds when they come into contact with airborne viruses. Most often, the virus spreads from person to person in respiratory droplets from sneezing or coughing. Transmission of viruses can also spread due to poor hand washing techniques as the virus can be passed from person to person by coming in contact with respiratory droplets from an infected person with a handshake, touching the nose, eyes, or mouth after coming in contact with the virus. Some viruses can live on surfaces such as sink faucets, door and drawer handles, table surfaces, pens, and computer keyboards for up to two hours.
People should understand that upper respiratory infections are contagious and are spread from person to person. Individuals are infected with the virus before symptoms arise and are therefore potentially contagious even before they know they are ill. Thus, hygienic measures such as covering sneezes and coughs, and regular hand washing should be a routine habit practiced by everyone even when not ill.
Rhinovirus (rhino from the Greek word for nose) and coronavirus are the two most common viruses causing upper respiratory infections. Other viruses including parainfluenza virus, respiratory syncytial virus, and adenovirus can cause colds but may also cause pneumonia, especially in infants and children.
More information on Nonspecific Upper Respiratory Tract Infection
https://www.uhs.uga.edu/healthtopics/respiratory.html
http://www.medicinenet.com/upper_respiratory_infection/article.htm
http://www.hopkinsmedicine.org/healthlibrary/conditions/pediatrics/upper_respiratory_infection_uri_or_common_cold_90,P02966/
http://www.emedicinehealth.com/upper_respiratory_infection/page2_em.htm#upper_respiratory_infection_causes
Sexually Transmitted Infections/Sexually Transmitted Diseases
Key facts
- More than 1 million people acquire a sexually transmitted infection (STI) every day.
- Each year, an estimated 500 million people become ill with one of 4 STIs: chlamydia, gonorrhoea, syphilis and trichomoniasis.
- More than 530 million people have the virus that causes genital herpes (HSV2).
- More than 290 million women have a human papillomavirus (HPV) infection.
- The majority of STIs are present without symptoms.
- Some STIs can increase the risk of HIV acquisition three-fold or more.
- STIs can have serious consequences beyond the immediate impact of the infection itself, through mother-to-child transmission of infections and chronic diseases.
- Drug resistance, especially for gonorrhoea, is a major threat to reducing the impact of STIs worldwide.
What are sexually transmitted infections and how are they transmitted?
STIs are caused by more than 30 different bacteria, viruses and parasites and are spread predominantly by sexual contact, including vaginal, anal and oral sex.
Some STIs may be spread via skin-to-skin sexual contact. The organisms causing STIs can also be spread through non-sexual means such as blood products and tissue transfer. Many STIs—including chlamydia, gonorrhoea, hepatitis B, HIV, HPV, HSV2 and syphilis—can also be transmitted from mother to child during pregnancy and childbirth.
A person can have an STI without having obvious symptoms of disease. Therefore, the term “sexually transmitted infection” is a broader term than “sexually transmitted disease” (STD). Common symptoms of STDs include vaginal discharge, urethral discharge in men, genital ulcers, and abdominal pain.
Eight of the more than 30 pathogens known to be transmitted through sexual contact have been linked to the greatest incidence of illness. Of these 8 infections, 4 are currently curable: syphilis, gonorrhoea, chlamydia and trichomoniasis. The other four are viral infections and are incurable, but can be mitigated or modulated through treatment: hepatitis B, herpes, HIV, and HPV.
STIs can have serious consequences beyond the immediate impact of the infection itself.
- Some STIs can increase the risk of HIV acquisition three-fold or more.
- Mother-to-child transmission of STIs can result in stillbirth, neonatal death, low-birth-weight and prematurity, sepsis, pneumonia, neonatal conjunctivitis, and congenital deformities. Syphilis in pregnancy leads to approximately 305,000 fetal and neonatal deaths every year and leaves 215,000 infants at increased risk of dying from prematurity, low-birth-weight or congenital disease.
- HPV infection causes 530,000 cases of cervical cancer and 275,000 cervical cancer deaths each year.
- STIs such as gonorrhoea and chlamydia are major causes of pelvic inflammatory disease, adverse pregnancy outcomes and infertility.
Prevention of STIs
Counselling and behavioral interventions offer primary prevention against STIs (including HIV), as well as against unintended pregnancies. These include:
- Comprehensive sexuality education, STI and HIV pre- and post-test counselling;
- Safer sex/risk-reduction counselling, condom promotion; and
- Interventions targeted at key and vulnerable populations, such as adolescents, sex workers, men who have sex with men and people who inject drugs.
- In addition, counselling can improve people’s ability to recognize the symptoms of STIs and increase the likelihood they will seek care or encourage a sexual partner to do so. Unfortunately, lack of public awareness, lack of training of health workers, and long-standing, widespread stigma around STIs remain barriers to greater and more effective use of these interventions.
Barrier methods
When used correctly and consistently, condoms offer one of the most effective methods of protection against STIs, including HIV. Female condoms are effective and safe, but are not used as widely by national programs as male condoms.
Diagnosis of STIs
The only inexpensive, rapid blood test currently available for an STI is for syphilis. This test is already in use in some resource-limited settings. The test is accurate, can provide results in 15 to 20 minutes, and is easy to use with minimal training. Rapid syphilis tests have been shown to increase the number of pregnant women tested for syphilis. However, increased efforts are still needed in most low- and middle-income countries to ensure that all pregnant women receive a syphilis test.
Several rapid tests for other STIs are under development and have the potential to improve STI diagnosis and treatment, especially in resource-limited settings.
Treatment of STIs
Three bacterial STIs (chlamydia, gonorrhea and syphilis) and one parasitic STI (trichomoniasis) are generally curable with existing, effective single-dose regimens of antibiotics.
For herpes and HIV, the most effective medications available are antivirals that can modulate the course of the disease, though they cannot cure the disease.
For hepatitis B, immune system modulators (interferon) and antiviral medications can help to fight the virus and slow damage to the liver.
Resistance of STIs—in particular gonorrhea—to antibiotics has increased rapidly in recent years and has reduced treatment options. The emergence of decreased susceptibility of gonorrhea to the “last line” treatment option (oral and injectable cephalosporin’s) together with antimicrobial resistance already shown to penicillin’s, sulphonamide’s, tetracycline’s, quinolones and macrolides make gonorrhea a multidrug-resistant organism. Antimicrobial resistance for other STIs, though less common, also exists, making prevention and prompt treatment critical.
For more information
http://www.who.int/mediacentre/factsheets/fs110/en/
http://www.nlm.nih.gov/medlineplus/sexuallytransmitteddiseases.html
There are many types of STD’s. Please visit http://www.cdc.gov/std/ for a list of them along with their signs and symptoms and prevention.
http://www.webmd.com/sexual-conditions/ss/slideshow-std-pictures-and-facts
Managing Stress: A Guide for College Students
There is no doubt that many college students feel stress. We may know we have stress when we experience it, but what is it exactly?
Stress is defined as a response to a demand that is placed upon you. Without some stress, people would not get a lot done. That extra burst of adrenaline that helps you finish your final paper, perform well in sports, or meet any challenge is positive stress. It is a short-term physiological tension and added mental alertness that subsides when the challenge has been met, enabling you to relax and carry on. Responses to stress can be physical, such as a headache; emotional, such as fear or sadness; and mental, such as increased anxiety. If you cannot return to a relaxed state, then the stress becomes negative. The changes in your body (increased heart rate, higher blood pressure and muscle tension) start to take their toll, often leading to mental and physical exhaustion and illness. Too much stress can cause problems and affect our health, productivity and relationships.
https://www.uhs.uga.edu/stress/index.html
http://www.pinterest.com/docorman/stress-images/
http://www.heart.org/HEARTORG/GettingHealthy/StressManagement/Stress-Management_UCM_001082_SubHomePage.jsp
The Most Stressed Out Generation? Young Adults. See more at:
http://healthland.time.com/2013/02/07/the-most-stressed-out-generation-young-adults/
http://www.nimh.nih.gov/health/publications/stress/index.shtml
